Retiree Prescription Drug Plan
Express Scripts provides prescription coverage, which is included with each of the medical plans.
Price your prescription
- Before you fill a prescription ask your doctor about your options. Generic prescriptions are usually less expensive than name-brand medications. You should also consult with your pharmacist about the cost, as many retailers offer generic discount programs that may save you more.
- All prescription costs filed with your insurance card will apply toward meeting your deductible.
- You can research the cost of prescriptions by logging in to your Express Scripts account at express-scripts.com.
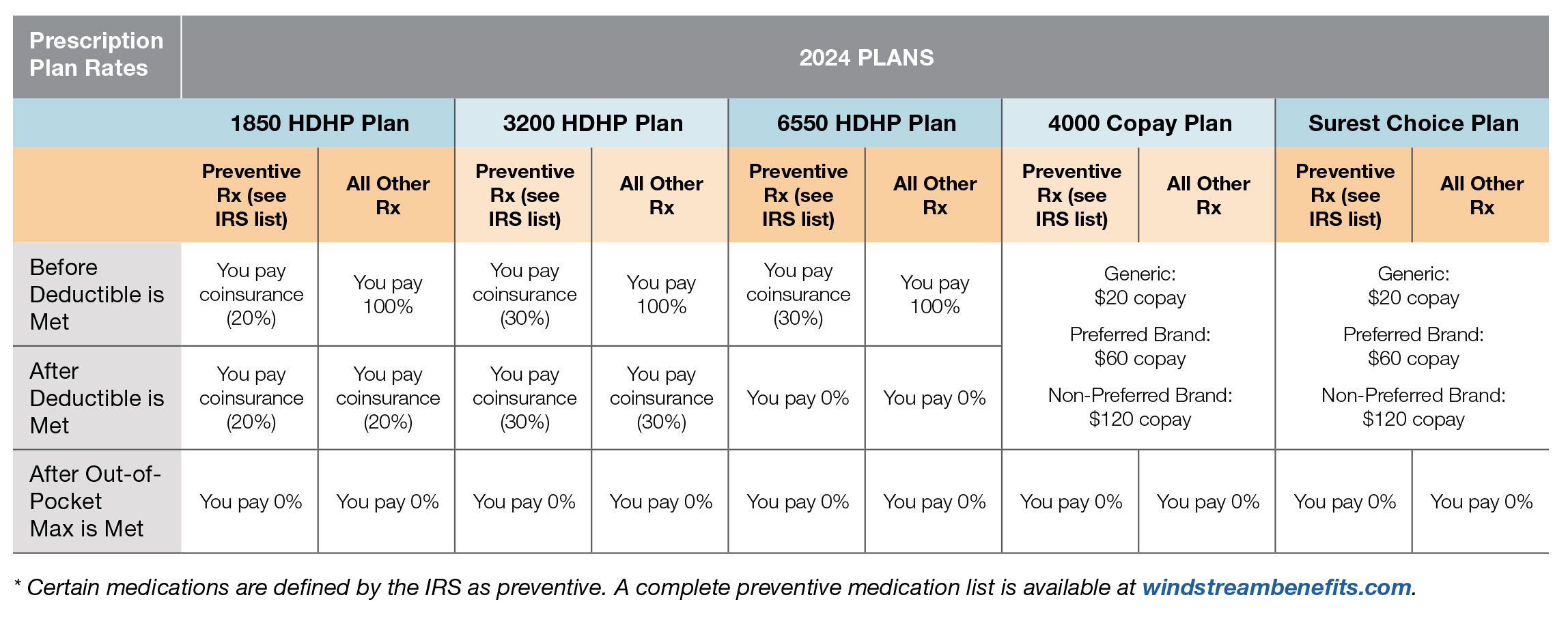
Prescription Plan Rates
 Filling a Prescription
Filling a Prescription
When you fill a prescription, you pay the retail price until you reach your deductible. Both medical and pharmacy expenses count toward meeting your deductible. After meeting your deductible, you pay your coinsurance rate until you reach the out-of-pocket maximum at which time Windstream pays 100% of the prescription cost.
You may fill up to a 30-day supply at a retail pharmacy. Maintenance medications must be filled via home delivery or using the Walgreens 90-day maintenance program after two orders have been filled at a retail pharmacy. The pharmacy network includes retailers such as Wal-Mart, Walgreens, Kroger, Costco, Safeway, Albertsons, and Rite-Aid.
Prior Authorization
Certain prescription drugs require prior authorization to confirm appropriateness of treatment. The prescribing physician should call Express Scripts before submission to the pharmacy to avoid delays and to expedite the authorization process. The list of medications requiring prior authorization is published by Express Scripts and available at express-scripts.com.
Step Therapy
Step Therapy is a drug protocol management tool used to ensure appropriate drug therapies for certain conditions. The Step Therapy program recommends using a less expensive treatment that is known to be safe and effective for most people – referred to as a first-line drug – prior to using a more expensive drug for the same condition. The Express Scripts system will alert your pharmacist that your medication requires prior authorization if you are trying to fill a prescription for a drug that is not identified as a first- line drug within a class that requires step therapy. If this occurs, you will need to contact your physician to either switch to a first-line drug or have your physician call Express Scripts for information on how to obtain a prior authorization for a second-line drug.
Specialty Medication
If you are using a specialty medication, you may fill it at a retail pharmacy initially. After that, you will need to order your medication through Accredo, Express Scripts’ specialty pharmacy. Specialty medications are those used for chronic or complex disease states such as: Hepatitis, Multiple Sclerosis, Growth Hormone Deficiency, Rheumatoid Arthritis, Infertility, Hemophilia, and Oncology.
Brand Exclusions
The Brand Exclusion program targets brand name medications that are not available as a generic. Instead, these brands have therapeutically equivalent generic alternatives available. Therapeutically equivalent means that these medications can be expected to produce essentially the same therapeutic outcomes. Brand exclusions are in place in the following therapy classes. If you choose a brand-name drug, you will be responsible for the full cost of the prescription even if you have met your deductible. Generic options are covered under the plan.
- Acne – topical with antibiotic
- Acne – topical
- Fenofibrates (e.g. for cholesterol treatment)
- Nasal antihistamines
- Nasal steroids
- Proton Pump Inhibitors (PPIs) (e.g. for gastric acid treatment)
- Statins (e.g. for cholesterol treatment)
- Sedative hypnotics
- Triptans (e.g. for migraine headaches)
In rare circumstances, use of the brand name may be medically necessary for treatment. In those cases, your physician may request a prior authorization by calling ExpressScripts at 866.804.7613.
Helpful Links |
